Fasting for IBS: Comprehensive Guide to Managing Irritable Bowel Syndrome
1. Introduction to Fasting for IBS
Fasting for IBS is an emerging approach that many individuals are exploring to manage their Irritable Bowel Syndrome symptoms. IBS is a common gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. Traditional treatments often include dietary modifications and medication, but fasting offers a different strategy that focuses on giving the digestive system regular breaks to reduce inflammation and promote gut health.
2. Benefits of Fasting for IBS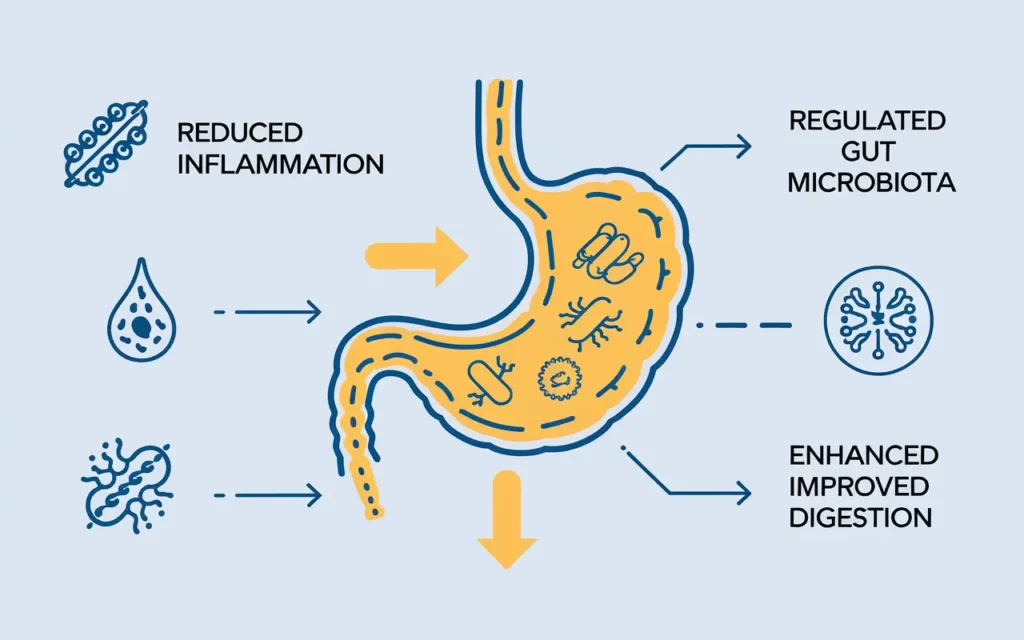
Fasting for IBS can provide several benefits that help alleviate the symptoms associated with the condition. By reducing the frequency of meals, fasting may decrease the digestive workload, allowing the gut to heal and reducing inflammation. Additionally, fasting can help regulate the gut microbiota, which plays a crucial role in digestive health and may influence IBS symptoms.
Improved Digestive Health
One of the primary benefits of fasting for IBS is the improvement in overall digestive health. Regular fasting periods can give the gastrointestinal tract time to rest and repair, potentially reducing the severity and frequency of IBS flare-ups.
Weight Management
Fasting for IBS can also aid in weight management. Many individuals with IBS struggle with maintaining a healthy weight due to dietary restrictions and digestive discomfort. Fasting can help regulate metabolism and support weight loss or maintenance.
Reduced Inflammation
Chronic inflammation is often linked to IBS symptoms. Fasting for IBS may help reduce inflammation by decreasing the production of pro-inflammatory cytokines, thereby alleviating pain and discomfort.
3. Scientific Research on Fasting for IBS
Fasting for IBS is supported by various scientific studies that explore its impact on the digestive system and gut health. Research indicates that fasting can modulate the gut microbiota, reduce intestinal permeability, and decrease inflammatory markers, all of which are beneficial for managing IBS symptoms.
Gut Microbiota Modulation
Studies have shown that fasting can alter the composition of the gut microbiota, promoting the growth of beneficial bacteria that aid in digestion and reduce inflammation. This modulation can help balance the gut environment, potentially alleviating IBS symptoms.
Intestinal Permeability
Fasting for IBS may help improve intestinal permeability, often referred to as “leaky gut.” By giving the gut time to repair, fasting can strengthen the intestinal barrier, preventing the passage of harmful substances that may trigger IBS symptoms.
Inflammatory Markers
Research indicates that fasting can lower levels of inflammatory markers in the body. Reduced inflammation can lead to decreased abdominal pain and discomfort, which are common symptoms of IBS.
4. Fasting Methods Suitable for IBS
Fasting for IBS involves selecting appropriate fasting methods that align with individual health needs and lifestyle. Not all fasting protocols are suitable for everyone, especially those with IBS, so it’s essential to choose methods that minimize stress on the digestive system.
Intermittent Fasting (IF)
Intermittent Fasting is one of the most popular fasting methods for IBS. It involves alternating periods of eating and fasting, such as the 16/8 method, where you fast for 16 hours and eat within an 8-hour window. This approach can help regulate digestion and reduce IBS symptoms.
Time-Restricted Eating (TRE)
Time-Restricted Eating limits food intake to specific hours of the day, such as eating only between 10 AM and 6 PM. This method can help synchronize eating patterns with the body’s natural circadian rhythms, potentially improving gut health and reducing IBS flare-ups.
Extended Fasting
Extended fasting involves fasting for periods longer than 24 hours, such as 48 or 72 hours. While this method can be more challenging, it may offer significant benefits for gut healing. However, it should be approached with caution and under medical supervision, especially for individuals with IBS.
Alternate-Day Fasting (ADF)
Alternate-Day Fasting involves alternating between fasting days and eating days. On fasting days, calorie intake is significantly reduced or completely abstained. This method can help reduce overall calorie intake and support weight management, which may indirectly benefit IBS symptoms.
5. Fasting Diet Plans for IBS Sufferers
Fasting for IBS can be effectively combined with specific diet plans to maximize symptom relief and improve digestive health. Tailoring your diet to support fasting protocols is crucial for managing IBS effectively.
Low-FODMAP Diet
The Low-FODMAP diet restricts fermentable carbohydrates that can exacerbate IBS symptoms. Combining this diet with fasting can help reduce bloating, gas, and abdominal pain.
Anti-Inflammatory Diet
An anti-inflammatory diet focuses on foods that reduce inflammation in the body. Incorporating anti-inflammatory foods during eating periods can complement fasting for IBS by further reducing intestinal inflammation.
Balanced Macronutrient Intake
Ensuring a balanced intake of proteins, carbohydrates, and fats during eating periods is essential. A balanced diet supports overall health and provides the necessary nutrients for gut repair and function.
Hydration and Electrolyte Balance
Maintaining proper hydration and electrolyte balance is critical, especially during fasting periods. Adequate fluid intake helps prevent constipation and supports overall digestive health.
Sample Fasting Diet Plan for IBS
| Time | Meal | Description |
|---|---|---|
| 6:00 AM | Breakfast | Low-FODMAP smoothie with spinach, banana, and lactose-free yogurt. |
| 12:00 PM | Lunch | Grilled chicken salad with mixed greens, carrots, and a lemon vinaigrette. |
| 3:00 PM | Snack | Rice cakes with almond butter and sliced strawberries. |
| 7:00 PM | Dinner | Baked salmon with quinoa and steamed zucchini. |
6. Personal Stories: Overcoming IBS with Fasting
Fasting for IBS has helped many individuals manage their symptoms and improve their quality of life. Personal stories provide valuable insights into the practical application of fasting and its impact on daily living.
Jane’s Journey
Jane struggled with severe IBS symptoms for years. After incorporating intermittent fasting into her routine, she noticed a significant reduction in bloating and abdominal pain. Jane credits fasting for giving her digestive system the rest it needed to heal.
Mark’s Transformation
Mark found traditional IBS treatments ineffective. He decided to try time-restricted eating and experienced fewer flare-ups and improved bowel regularity. Mark emphasizes the importance of consistency and listening to his body’s signals during fasting periods.
Emily’s Success
Emily combined fasting with a Low-FODMAP diet and saw remarkable improvements in her IBS symptoms. She appreciates the structured approach that fasting provides, allowing her to better manage her dietary intake and digestive health.
7. Expert Opinions on Fasting for IBS
Fasting for IBS has garnered attention from medical professionals and nutrition experts. Their insights provide a balanced perspective on the effectiveness and safety of fasting as a treatment option.
Gastroenterologist Insights
Dr. Sarah Thompson, a gastroenterologist, states, “Fasting for IBS can be beneficial for some patients, particularly when combined with dietary modifications. However, it’s essential to approach fasting cautiously and under medical supervision to avoid potential nutrient deficiencies.”
Nutritionist Recommendations
Nutritionist John Davis advises, “Fasting for IBS should be personalized. It’s important to identify which fasting method suits an individual’s lifestyle and health condition. Incorporating nutrient-dense foods during eating periods is crucial to support gut health.”
Psychologist’s Perspective
Dr. Lisa Martinez, a clinical psychologist, adds, “The psychological aspect of fasting should not be overlooked. Individuals with IBS often experience stress-related symptoms, and mindful fasting practices can help reduce anxiety and improve overall well-being.”
8. Fasting vs. Traditional IBS Treatments
Fasting for IBS offers an alternative to traditional treatments, each with its own set of advantages and limitations. Understanding the differences can help individuals make informed decisions about their IBS management strategies.
Fasting vs. Medication
While medications can provide immediate relief from IBS symptoms, they often come with side effects and may not address the underlying causes. Fasting, on the other hand, focuses on improving gut health and reducing inflammation without the use of drugs.
Fasting vs. Dietary Changes
Dietary changes, such as adopting a Low-FODMAP diet, are commonly recommended for IBS sufferers. Combining fasting with these dietary modifications can enhance the effectiveness of symptom management by providing the digestive system with regular breaks.
Fasting vs. Behavioral Therapies
Behavioral therapies, including stress management and cognitive-behavioral therapy, are essential for managing IBS. Fasting can complement these therapies by reducing physical symptoms, thereby supporting mental well-being.
Comparison Table: Fasting vs. Traditional Treatments
| Aspect | Fasting for IBS | Traditional Treatments |
|---|---|---|
| Approach | Dietary and fasting protocols to support gut health | Medications and dietary supplements |
| Benefits | Reduces inflammation, improves gut microbiota | Immediate symptom relief |
| Side Effects | Potential nutrient deficiencies if not managed properly | Possible gastrointestinal and systemic side effects |
| Sustainability | Requires lifestyle adjustments and consistency | Depends on long-term medication use |
9. Gut Health and Fasting: Understanding the Connection
Fasting for IBS is closely linked to gut health, as the gut microbiota plays a pivotal role in digestive processes and overall well-being. Understanding this connection is essential for leveraging fasting to manage IBS effectively.
Role of Gut Microbiota
The gut microbiota consists of trillions of microorganisms that aid in digestion, produce essential nutrients, and regulate the immune system. Imbalances in the gut microbiota can lead to increased inflammation and IBS symptoms.
Fasting’s Impact on Gut Microbiota
Fasting for IBS can help rebalance the gut microbiota by promoting the growth of beneficial bacteria and reducing harmful strains. This shift can enhance digestive function and reduce symptoms like bloating and pain.
Maintaining a Healthy Gut During Fasting
To maintain gut health during fasting periods, it’s important to consume probiotic-rich foods during eating windows and stay hydrated. Additionally, incorporating prebiotic fibers can support the growth of beneficial bacteria.
Tips for Maintaining Gut Health While Fasting
- Stay Hydrated: Drink plenty of water to support digestion and prevent constipation.
- Consume Probiotics: Include yogurt, kefir, and fermented vegetables in your diet.
- Eat Prebiotics: Foods like garlic, onions, and bananas help nourish beneficial gut bacteria.
- Avoid Trigger Foods: Identify and eliminate foods that exacerbate IBS symptoms.
10. Potential Risks of Fasting for IBS Patients
While fasting for IBS can offer numerous benefits, it is not without potential risks. It’s important to be aware of these risks to ensure that fasting is approached safely and effectively.
Nutrient Deficiencies
Extended fasting periods without proper planning can lead to deficiencies in essential nutrients, such as vitamins, minerals, and proteins, which are vital for overall health and gut function.
Exacerbation of Symptoms
In some cases, fasting may initially worsen IBS symptoms, such as increased abdominal pain or changes in bowel habits. It’s crucial to monitor symptoms and adjust fasting protocols as needed.
Disordered Eating Patterns
Fasting can sometimes lead to unhealthy relationships with food, particularly for individuals prone to disordered eating. It’s important to approach fasting with mindfulness and seek professional guidance if needed.
Dehydration
Inadequate fluid intake during fasting periods can result in dehydration, which may exacerbate IBS symptoms and negatively impact overall health.
Safety Tips for Fasting with IBS
- Consult a Healthcare Professional: Always seek medical advice before starting a fasting regimen.
- Start Slowly: Gradually incorporate fasting into your routine to allow your body to adjust.
- Monitor Symptoms: Keep track of your IBS symptoms and adjust your fasting plan accordingly.
- Ensure Nutrient Intake: Focus on nutrient-dense foods during eating periods to prevent deficiencies.
11. Conclusion
Fasting for IBS presents a promising alternative to traditional treatment methods, offering potential benefits such as improved gut health, reduced inflammation, and better symptom management. However, it is essential to approach fasting with careful planning and professional guidance to mitigate potential risks. By integrating fasting with appropriate dietary strategies and maintaining a focus on overall well-being, individuals with IBS can achieve better control over their symptoms and enhance their quality of life.
12. References
For further reading and authoritative information on fasting for IBS, please refer to the following sources: