Comprehensive Guide to a Diverticulosis Diet Plan
Table of Contents
- 1. Introduction to Diverticulosis Diet Plan
- 2. Understanding Diverticulosis
- 3. Importance of a Diverticulosis Diet Plan
- 4. High-Fiber Foods in Your Diet Plan
- 5. Foods to Avoid in a Diverticulosis Diet Plan
- 6. Meal Planning Strategies
- 7. Hydration Tips for Diverticulosis
- 8. Delicious Recipes for Your Diet Plan
- 9. Common Mistakes and How to Avoid Them
- 10. Maintaining Your Diverticulosis Diet Plan Long-Term
- 11. Additional Resources
- 12. Frequently Asked Questions
1. Introduction to Diverticulosis Diet Plan
Diverticulosis diet plan is essential because it plays a pivotal role in managing and preventing complications associated with diverticulosis. By adhering to a well-structured diet, individuals can alleviate symptoms, reduce the risk of flare-ups, and improve overall digestive health.
What is Diverticulosis?
Diverticulosis is a condition characterized by the formation of small pouches, called diverticula, in the walls of the colon. These pouches develop when weak spots in the colon give way under pressure, causing sections to bulge out. While diverticulosis itself often doesn’t cause symptoms, it can lead to more severe conditions like diverticulitis if not managed properly.
Prevalence and Demographics
Diverticulosis is more common in older adults, particularly those over the age of 40. Lifestyle factors such as diet, physical activity, and overall health also play significant roles in its development. Understanding the demographics helps in tailoring the diverticulosis diet plan to meet the specific needs of different age groups and lifestyles.
2. Understanding Diverticulosis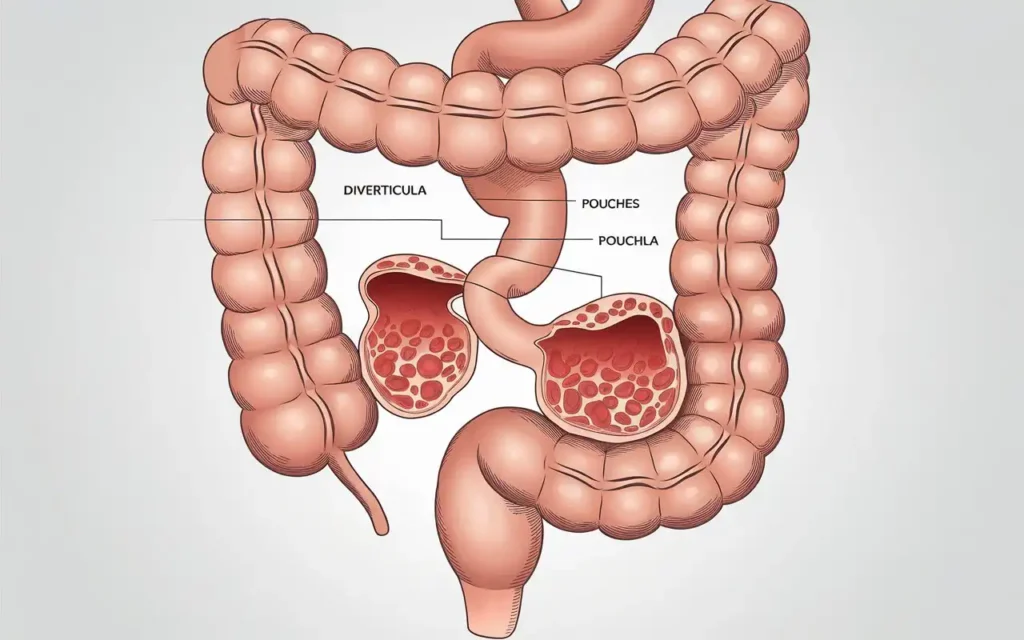
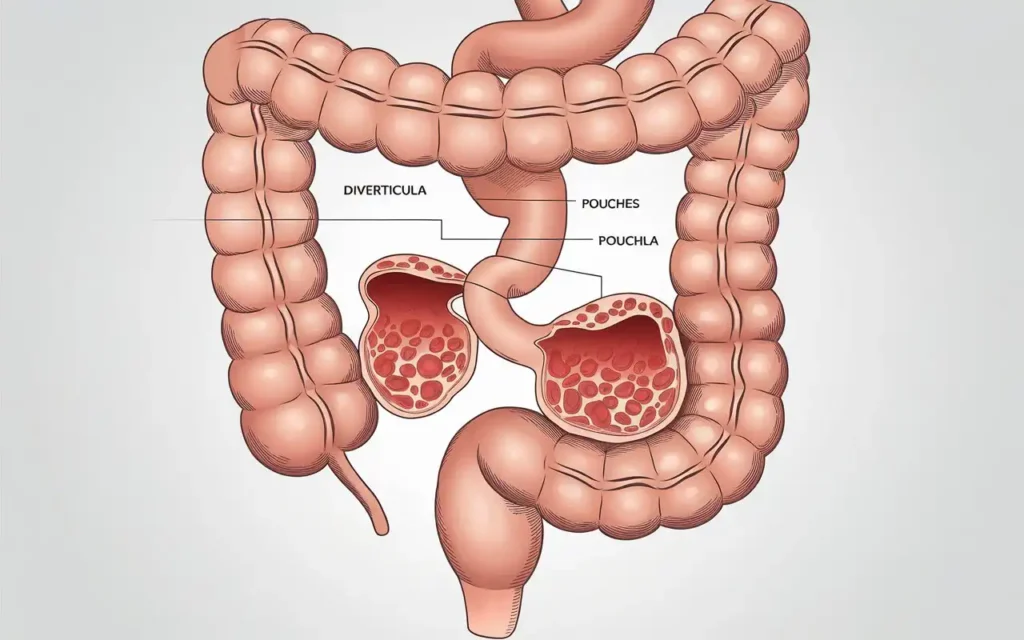
Diverticulosis diet plan begins with a thorough understanding of the condition itself. Diverticula are small, bulging pouches that can form in the digestive tract, particularly in the colon. These pouches can become inflamed or infected, leading to a more severe condition known as diverticulitis.
Causes and Risk Factors
- Low-fiber diet: A diet lacking in fiber leads to harder stools and increased pressure in the colon.
- Age: More common in individuals over 40 due to changes in the colon’s structure over time.
- Obesity: Excess body weight increases the pressure on the colon.
- Lack of physical activity: Regular exercise helps maintain bowel health.
- Smoking: Linked to a higher risk of developing diverticulosis.
Symptoms and Complications
While diverticulosis is often asymptomatic, some individuals may experience:
- Abdominal pain, typically on the lower left side
- Bloating and gas
- Constipation or, less commonly, diarrhea
- Fever and nausea if complications like diverticulitis occur
Diagnosis
Diverticulosis is usually diagnosed through a colonoscopy, which allows doctors to view the inside of the colon and identify diverticula. Other diagnostic tools include CT scans, which can detect inflammation or infection in the diverticula.
3. Importance of a Diverticulosis Diet Plan
Diverticulosis diet plan is crucial as it helps in managing symptoms, preventing complications, and promoting overall gut health. A balanced diet rich in fiber can soften stool, making it easier to pass and reducing pressure in the colon.
Role of Fiber in Digestive Health
Fiber is indispensable in a diverticulosis diet plan because it adds bulk to the stool and facilitates smoother bowel movements. There are two main types of fiber:
- Soluble Fiber: Dissolves in water to form a gel-like substance. It helps lower blood cholesterol and glucose levels.
- Insoluble Fiber: Does not dissolve in water and helps move material through the digestive system.
Benefits of a Proper Diet Plan
- Reduces the risk of diverticulitis by preventing stool hardening and subsequent colon pressure.
- Alleviates digestive discomfort such as bloating and constipation.
- Promotes regular bowel movements, contributing to overall colon health.
- Enhances overall nutritional intake, supporting overall health and well-being.
Impact on Quality of Life
A well-maintained diverticulosis diet plan can significantly improve an individual’s quality of life by minimizing symptoms, reducing the need for medical interventions, and fostering a sense of control over one’s health.
4. High-Fiber Foods in Your Diet Plan
Diverticulosis diet plan emphasizes the inclusion of high-fiber foods to ensure proper digestion and prevent the formation of diverticula. Fiber adds bulk to the stool and facilitates smoother bowel movements.
Soluble vs. Insoluble Fiber
| Soluble Fiber | Insoluble Fiber |
|---|---|
| Oats, barley, nuts, seeds, beans, lentils, and some fruits and vegetables. | Whole grains, wheat bran, vegetables, and nuts. |
Top High-Fiber Foods to Include
- Whole Grains: Brown rice, quinoa, barley, and whole wheat products.
- Fruits: Apples, pears, berries, oranges, and bananas.
- Vegetables: Broccoli, carrots, leafy greens, Brussels sprouts, and sweet potatoes.
- Legumes: Beans, lentils, chickpeas, and peas.
- Nuts and Seeds: Almonds, chia seeds, flaxseeds, and sunflower seeds.
Incorporating Fiber into Your Diet
Gradually increase fiber intake to allow your digestive system to adjust. Start by adding a small portion of high-fiber foods to each meal and increase the quantity over time. This helps prevent bloating and gas.
Benefits of Specific High-Fiber Foods
- Oats: Rich in beta-glucan, a type of soluble fiber that helps lower cholesterol levels.
- Apples: Contain pectin, a soluble fiber that aids in digestion.
- Broccoli: High in insoluble fiber, promoting regular bowel movements.
- Beans: Packed with both soluble and insoluble fiber, supporting overall digestive health.
5. Foods to Avoid in a Diverticulosis Diet Plan
While a diverticulosis diet plan focuses on high-fiber foods, it’s equally important to avoid certain foods that can exacerbate symptoms or lead to complications. Avoiding these foods helps maintain colon health and prevents unnecessary strain.
Common Foods to Eliminate
- Red Meat and Processed Meats: High in fat and can increase the risk of diverticulitis.
- Refined Grains and Sugary Foods: Lack fiber and can lead to spikes in blood sugar levels.
- Fried and Fatty Foods: Difficult to digest and can cause discomfort.
- Seeds and Nuts: Previously thought to cause diverticula to become inflamed, though recent studies are inconclusive. It’s best to consult with a healthcare provider.
- Spicy Foods: May irritate the digestive tract and exacerbate symptoms.
Impact of Avoided Foods on Diverticulosis
Eliminating these foods from your diverticulosis diet plan helps reduce inflammation, prevent flare-ups, and maintain a healthy digestive system. For instance, reducing red meat intake can lower the risk of developing diverticulitis, a painful complication of diverticulosis.
Alternatives to Avoided Foods
- Instead of Red Meat: Opt for lean proteins like chicken, turkey, or fish.
- Instead of Refined Grains: Choose whole grains such as brown rice, quinoa, or whole wheat bread.
- Instead of Fried Foods: Try baking, grilling, or steaming your meals.
- Instead of Spicy Foods: Use herbs and mild spices to flavor your dishes.
Individual Considerations
It’s important to note that dietary triggers can vary among individuals. Keeping a food diary can help identify specific foods that may worsen your symptoms, allowing you to tailor your diverticulosis diet plan accordingly.
6. Meal Planning Strategies
Effective diverticulosis diet plan requires thoughtful meal planning to ensure balanced nutrition and adherence to dietary guidelines. Proper meal planning helps in maintaining consistency, preventing impulsive eating, and ensuring that you receive all necessary nutrients.
Creating a Balanced Meal Plan
- Incorporate High-Fiber Foods: Ensure each meal includes sources of both soluble and insoluble fiber.
- Regular Meal Times: Eating at consistent times helps regulate bowel movements and prevent constipation.
- Balanced Macronutrients: Include a healthy balance of carbohydrates, proteins, and fats in each meal.
- Portion Control: Monitor portion sizes to avoid overeating, which can strain the digestive system.
Planning for Snacks
Healthy snacks can help maintain energy levels and prevent overeating during meals. Opt for fiber-rich snacks such as:
- Fresh fruit slices with nut butter
- Vegetable sticks with hummus
- Whole grain crackers with cheese
- Trail mix with nuts and dried fruits
Preparing Ahead of Time
Meal prepping can save time and ensure you always have healthy options available. Consider preparing the following in advance:
- Chopped vegetables for salads and snacks
- Cooked grains like quinoa or brown rice
- Portioned servings of legumes and beans
- Homemade soups and stews
Sample Weekly Meal Plan
| Day | Breakfast | Lunch | Dinner | Snacks |
|---|---|---|---|---|
| Monday | Oatmeal with berries and chia seeds | Quinoa salad with mixed vegetables and chickpeas | Grilled chicken breast with steamed broccoli and sweet potatoes | Apple slices with almond butter |
| Tuesday | Whole grain toast with avocado and poached eggs | Lentil soup with a side of whole wheat bread | Baked salmon with quinoa and asparagus | Carrot sticks with hummus |
| Wednesday | Greek yogurt with granola and fresh fruit | Spinach and feta stuffed whole wheat pita | Stir-fried tofu with mixed vegetables and brown rice | Handful of mixed nuts |
7. Hydration Tips for Diverticulosis
A proper diverticulosis diet plan isn’t complete without adequate hydration. Water helps fiber do its job effectively by softening the stool and preventing constipation.
Recommended Fluids
- Water: The best choice for staying hydrated.
- Herbal Teas: Calming and can aid in digestion.
- Clear Broths: Provide hydration and essential nutrients.
- 100% Fruit Juices (in moderation): Offer vitamins but should be limited due to sugar content.
Daily Hydration Goals
Aim to drink at least 8 glasses (64 ounces) of water per day. Adjust based on activity level, climate, and individual needs. Listening to your body’s thirst cues is also important.
Signs of Dehydration
- Dark yellow urine
- Dry mouth and lips
- Fatigue and dizziness
- Headaches
Tips to Increase Fluid Intake
- Carry a reusable water bottle throughout the day.
- Set reminders to drink water regularly.
- Infuse water with fruits like lemon, lime, or berries for added flavor.
- Drink a glass of water before each meal.
8. Delicious Recipes for Your Diet Plan
Incorporating tasty recipes into your diverticulosis diet plan makes adherence enjoyable and sustainable. Below are some high-fiber, easy-to-prepare recipes that cater to various tastes and dietary preferences.
High-Fiber Breakfast: Berry Oatmeal
- 1 cup rolled oats
- 2 cups water or milk
- 1 cup mixed berries (blueberries, strawberries, raspberries)
- 1 tablespoon honey or maple syrup
- 1 tablespoon chia seeds (optional)
Instructions: In a saucepan, bring water or milk to a boil. Add rolled oats and reduce heat to simmer. Cook for about 5 minutes, stirring occasionally. Once thickened, remove from heat and stir in chia seeds if using. Top with mixed berries and drizzle with honey or maple syrup.
Lunch: Quinoa and Vegetable Salad
- 1 cup cooked quinoa
- 1 cup chopped vegetables (cucumbers, tomatoes, bell peppers)
- 1/2 cup chickpeas, rinsed and drained
- 2 tablespoons olive oil
- 1 tablespoon lemon juice
- Salt and pepper to taste
- Fresh herbs (parsley, cilantro) for garnish
Instructions: In a large bowl, combine cooked quinoa, chopped vegetables, and chickpeas. In a small bowl, whisk together olive oil, lemon juice, salt, and pepper. Pour the dressing over the salad and toss to combine. Garnish with fresh herbs before serving.
Dinner: Grilled Chicken with Steamed Broccoli and Sweet Potatoes
- 2 chicken breasts
- 1 tablespoon olive oil
- Salt, pepper, and your choice of herbs (rosemary, thyme)
- 2 cups broccoli florets
- 2 medium sweet potatoes, peeled and cubed
Instructions: Preheat the grill to medium-high heat. Rub the chicken breasts with olive oil, salt, pepper, and herbs. Grill the chicken for about 6-7 minutes on each side or until fully cooked. Meanwhile, steam the broccoli florets until tender. Boil the sweet potatoes until soft, then drain and serve alongside the grilled chicken and broccoli.
Snack: Apple Slices with Almond Butter
- 1 apple, sliced
- 2 tablespoons almond butter
Instructions: Arrange apple slices on a plate and serve with a side of almond butter for dipping.
Vegetarian Option: Lentil and Spinach Stew
- 1 cup dried lentils, rinsed
- 1 onion, chopped
- 2 cloves garlic, minced
- 2 cups spinach leaves
- 4 cups vegetable broth
- 1 tablespoon olive oil
- 1 teaspoon cumin
- Salt and pepper to taste
Instructions: In a large pot, heat olive oil over medium heat. Add chopped onion and garlic, sautéing until translucent. Add lentils, cumin, salt, and pepper, stirring to combine. Pour in vegetable broth and bring to a boil. Reduce heat and simmer for about 25 minutes or until lentils are tender. Stir in spinach leaves and cook until wilted. Serve hot.
Vegan Option: Chickpea and Avocado Wrap
- 1 can chickpeas, rinsed and drained
- 1 avocado, mashed
- 1/4 cup red onion, finely chopped
- 1 tablespoon lemon juice
- Salt and pepper to taste
- Whole wheat tortillas
- Fresh spinach leaves
Instructions: In a bowl, mash the chickpeas and avocado together. Mix in red onion, lemon juice, salt, and pepper. Spread the mixture onto whole wheat tortillas, add fresh spinach leaves, and roll up tightly. Slice in half and serve.
9. Common Mistakes and How to Avoid Them
Adhering to a diverticulosis diet plan can be challenging. Being aware of common mistakes helps in maintaining an effective diet and avoiding setbacks.
Sudden Increase in Fiber Intake
One of the most common mistakes is increasing fiber intake too quickly. This can lead to bloating, gas, and abdominal discomfort. To avoid this, gradually incorporate high-fiber foods into your diet over a few weeks, allowing your digestive system to adjust.
Inadequate Hydration
Not drinking enough water can counteract the benefits of a high-fiber diet, leading to constipation and increased colon pressure. Ensure you’re meeting your daily hydration goals by drinking at least 8 glasses of water each day.
Ignoring Individual Tolerances
Everyone’s digestive system responds differently to various foods. Some high-fiber foods may cause discomfort or exacerbate symptoms. Pay attention to your body’s signals and adjust your diet plan accordingly. Keeping a food diary can help identify which foods work best for you.
Overreliance on Supplements
While fiber supplements can be beneficial, they shouldn’t replace natural food sources. Whole foods provide a range of nutrients that supplements cannot offer. Use supplements as an adjunct to, not a substitute for, a balanced diverticulosis diet plan.
Neglecting Physical Activity
Physical activity complements a high-fiber diet by promoting regular bowel movements and overall digestive health. Incorporate regular exercise into your routine to enhance the effectiveness of your diet plan.
Skipping Meals
Skipping meals can lead to irregular bowel movements and increased pressure in the colon. Maintain a consistent eating schedule to support digestive health and prevent constipation.
Not Seeking Professional Guidance
Attempting to manage diverticulosis without professional advice can lead to ineffective or harmful dietary choices. Consult with a healthcare provider or a registered dietitian to develop a personalized diverticulosis diet plan that meets your specific needs.
10. Maintaining Your Diverticulosis Diet Plan Long-Term
Maintaining a diverticulosis diet plan requires commitment and lifestyle adjustments. Here are strategies to ensure long-term success and prevent relapse.
Consistency is Key
Sticking to your meal plans and making fiber-rich foods a staple in your diet helps prevent flare-ups and maintain digestive health. Consistency ensures that your body continually benefits from the positive effects of a high-fiber diet.
Regular Monitoring
Keep track of your symptoms and dietary intake. Monitoring allows you to identify patterns, recognize triggers, and make necessary adjustments to your diet plan. Tools such as food diaries or mobile apps can aid in tracking your progress.
Seek Support
Joining support groups or consulting with a dietitian can provide motivation and personalized advice. Sharing experiences with others facing similar challenges can offer emotional support and practical tips for maintaining your diet plan.
Adaptability
Life circumstances can change, and your diverticulosis diet plan may need adjustments. Whether you’re traveling, attending social events, or experiencing changes in your health, being adaptable ensures that you can maintain your diet plan under various conditions.
Education and Awareness
Stay informed about the latest research and recommendations related to diverticulosis and dietary management. Continuous learning empowers you to make informed decisions and refine your diet plan as needed.
Incorporate Variety
Including a wide range of high-fiber foods prevents dietary monotony and ensures a diverse intake of essential nutrients. Variety keeps meals interesting and satisfying, making it easier to adhere to your diet plan.
Celebrate Milestones
Recognize and celebrate your progress, no matter how small. Celebrating milestones fosters a positive relationship with your diet plan and reinforces your commitment to maintaining it long-term.
11. Additional Resources
For more information and support on managing diverticulosis through diet, consider exploring the following resources:
- Mayo Clinic on Diverticulosis
- WebMD Diverticulosis Diet
- National Institutes of Health: Diverticular Disease
- Healthline Diverticulosis Diet Guide
12. Frequently Asked Questions
1. Can I include dairy in my diverticulosis diet plan?
Yes, dairy products can be included in moderation. Opt for low-fat or non-dairy alternatives if you are lactose intolerant or if dairy seems to exacerbate your symptoms.
2. How quickly should I transition to a high-fiber diet?
Gradually increase your fiber intake over a few weeks to allow your digestive system to adjust. Sudden increases can cause bloating and gas.
3. Are there any supplements that can aid my diverticulosis diet plan?
Fiber supplements like psyllium husk can be beneficial, but they should complement, not replace, natural high-fiber foods. Always consult with a healthcare provider before starting any supplements.
4. Can exercise help manage diverticulosis?
Yes, regular physical activity promotes regular bowel movements and overall digestive health, complementing your diverticulosis diet plan.
5. Is it safe to follow a diverticulosis diet plan during pregnancy?
Generally, yes. However, it’s essential to consult with a healthcare provider to ensure that your diet plan meets the nutritional needs of both you and your baby.
6. How can I manage diverticulosis while traveling?
Plan ahead by researching restaurants that offer high-fiber options, packing healthy snacks, and staying hydrated. Maintaining your meal schedule as much as possible also helps.
7. What should I do if I experience a diverticulosis flare-up?
If you experience severe symptoms, consult with a healthcare provider immediately. During a flare-up, a temporary low-fiber or clear liquid diet may be recommended to allow the colon to heal.
8. Can I still enjoy desserts on a diverticulosis diet plan?
Yes, desserts can be included in moderation. Opt for high-fiber options like fruit-based desserts or those made with whole grains and natural sweeteners.
9. How does weight affect diverticulosis?
Obesity is a risk factor for diverticulosis. Maintaining a healthy weight through a balanced diet and regular exercise can reduce the risk of developing diverticula and related complications.
10. Should I avoid all nuts and seeds?
Recent studies suggest that nuts and seeds do not significantly increase the risk of diverticulitis. However, some individuals may find them irritating during flare-ups. It’s best to consult with your healthcare provider.
External References
- Mayo Clinic on Diverticulosis
- WebMD Diverticulosis Diet
- National Institutes of Health: Diverticular Disease
- Healthline Diverticulosis Diet Guide