Comprehensive Guide to a Congestive Heart Failure Diet
1. Understanding Congestive Heart Failure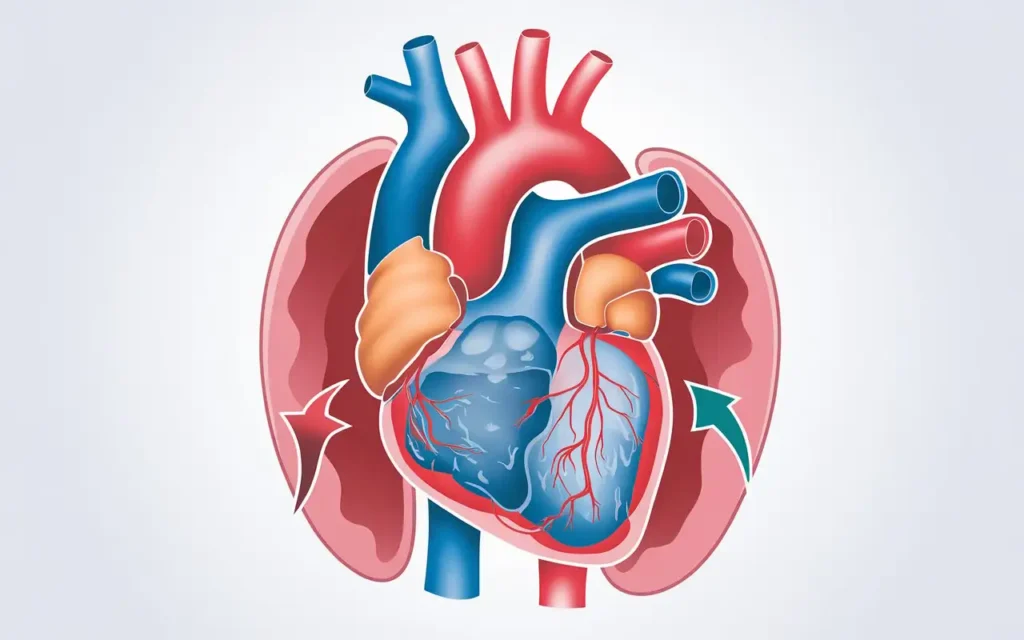
The congestive heart failure diet is essential because it plays a pivotal role in managing the symptoms and progression of congestive heart failure (CHF). CHF is a chronic condition where the heart struggles to pump blood effectively, leading to fluid buildup in various parts of the body.
What is Congestive Heart Failure?
Congestive heart failure is a condition characterized by the heart’s inability to pump sufficient blood to meet the body’s needs. This can result from weakened heart muscles, stiffened heart chambers, or other underlying heart conditions. CHF doesn’t mean that the heart has stopped working, but rather that it isn’t functioning optimally.
Causes and Risk Factors
- Coronary Artery Disease: The most common cause, where narrowed arteries reduce blood flow to the heart muscle.
- High Blood Pressure: Puts extra strain on the heart, leading to hypertrophy and eventual heart failure.
- Diabetes: Increases the risk of heart disease and can directly damage the heart muscle.
- Obesity: Excess weight forces the heart to work harder, increasing the risk of heart failure.
- Smoking: Damages blood vessels and reduces oxygen supply to the heart.
- Other Conditions: Such as valvular heart disease, arrhythmias, and cardiomyopathies.
Symptoms of CHF
- Shortness of Breath: Especially during physical activities or when lying down.
- Fatigue: Persistent tiredness and lack of energy.
- Swelling: In the legs, ankles, feet, abdomen, or other parts of the body due to fluid retention.
- Rapid or Irregular Heartbeat: Palpitations or a sensation of the heart racing.
- Persistent Cough or Wheezing: Often producing white or pink blood-tinged mucus.
- Increased Need to Urinate at Night: Due to fluid redistribution while lying down.
Stages of CHF
Understanding the stages of CHF can help in managing the condition effectively:
- Stage A: At high risk for developing heart failure but without structural heart disease or symptoms.
- Stage B: Structural heart disease is present but without signs or symptoms of heart failure.
- Stage C: Structural heart disease with prior or current symptoms of heart failure.
- Stage D: Refractory heart failure requiring specialized interventions.
Diagnosis and Monitoring
Early diagnosis and regular monitoring are crucial for managing CHF. Diagnostic methods include:
- Physical Examination: Checking for signs like swelling and listening for abnormal heart sounds.
- Imaging Tests: Such as echocardiograms, X-rays, and MRIs to assess heart function and structure.
- Blood Tests: To measure levels of natriuretic peptides, kidney function, and other markers.
- Electrocardiogram (ECG): To detect arrhythmias and other electrical issues.
Prognosis and Management
With appropriate management, many individuals with CHF can lead active lives. Management strategies include medication, lifestyle changes, dietary modifications, and in some cases, surgical interventions like implantable devices or heart transplants.
2. Importance of Diet in Managing CHF
The congestive heart failure diet is essential because it directly influences the body’s fluid balance, electrolyte levels, and overall heart health. Proper dietary management can alleviate symptoms, prevent hospitalizations, and improve quality of life for CHF patients.
Dietary Goals for CHF
- Reduce Sodium Intake: To prevent fluid retention and lower blood pressure.
- Control Fluid Consumption: To manage swelling and reduce the burden on the heart.
- Maintain Balanced Nutrient Intake: Ensuring adequate vitamins, minerals, and macronutrients.
- Manage Weight: Preventing obesity to reduce the heart’s workload.
- Optimize Electrolyte Levels: Balancing potassium, magnesium, and calcium for heart function.
Benefits of a CHF-Friendly Diet
Adhering to a CHF diet can help in reducing fluid retention, lowering blood pressure, and decreasing the heart’s workload. This leads to improved cardiac function and reduced risk of exacerbations. Additionally, a heart-healthy diet can enhance energy levels, support weight management, and improve overall well-being.
Impact on Medication Efficacy
A well-planned diet can enhance the effectiveness of CHF medications. For example, reducing sodium can complement diuretic therapy, while adequate potassium intake can support the use of ACE inhibitors or ARBs.
Long-Term Health Benefits
Beyond managing CHF, a heart-healthy diet reduces the risk of other chronic diseases such as diabetes, hypertension, and stroke. It promotes longevity and a higher quality of life by fostering overall cardiovascular health.
3. Key Nutrients for a CHF Diet

The congestive heart failure diet emphasizes specific nutrients that support heart health and overall well-being. Understanding these nutrients is crucial for effective dietary planning.
Sodium
Reducing sodium is paramount in a CHF diet to prevent fluid retention and lower blood pressure. High sodium intake can lead to increased blood volume, which strains the heart and exacerbates CHF symptoms.
- Recommended Intake: Generally less than 2,000 mg per day, but individual needs may vary.
- Sources of Sodium: Processed foods, canned soups, deli meats, snack foods, and restaurant meals.
Potassium
Potassium helps balance fluids and supports proper muscle function, including the heart. It works in tandem with sodium to regulate blood pressure and maintain electrolyte balance.
- Recommended Intake: Approximately 3,500-4,700 mg per day, depending on individual needs and medical advice.
- Sources of Potassium: Bananas, oranges, potatoes, spinach, and tomatoes.
Magnesium
Magnesium plays a role in maintaining normal heart rhythms and preventing arrhythmias. It’s also essential for muscle and nerve function.
- Recommended Intake: About 310-420 mg per day for adults.
- Sources of Magnesium: Whole grains, nuts, seeds, legumes, and leafy green vegetables.
Fiber
Dietary fiber aids in digestion and helps manage cholesterol levels, contributing to heart health. It also promotes satiety, aiding in weight management.
- Recommended Intake: 25-30 grams per day from food, not supplements.
- Sources of Fiber: Fruits, vegetables, whole grains, legumes, and nuts.
Omega-3 Fatty Acids
Omega-3s are essential for reducing inflammation and supporting cardiovascular function. They can help lower triglyceride levels and reduce the risk of arrhythmias.
- Recommended Intake: At least two servings of fatty fish per week.
- Sources of Omega-3s: Salmon, mackerel, sardines, flaxseeds, and walnuts.
Calcium
Calcium is vital for muscle function, including the heart muscle. It works with magnesium and potassium to maintain a healthy heart rhythm.
- Recommended Intake: 1,000 mg per day for most adults.
- Sources of Calcium: Dairy products, fortified plant-based milks, leafy greens, and tofu.
Vitamin D
Vitamin D supports bone health and may play a role in cardiovascular health by modulating inflammation and immune function.
- Recommended Intake: 600-800 IU per day, depending on age and health status.
- Sources of Vitamin D: Sunlight exposure, fortified foods, fatty fish, and supplements.
Protein
Adequate protein intake is necessary for maintaining muscle mass and overall bodily functions. It also supports tissue repair and immune function.
- Recommended Intake: Varies based on activity level, age, and overall health, typically 46-56 grams per day for adults.
- Sources of Protein: Lean meats, poultry, fish, beans, lentils, tofu, and low-fat dairy products.
4. Sodium Restriction Strategies

The congestive heart failure diet requires careful management of sodium intake to control fluid retention and blood pressure.
Understanding Sodium Labels
Learn how to read and interpret sodium content on food labels to make informed choices. Foods are often labeled with “low sodium,” “reduced sodium,” or “no salt added,” each indicating different levels of sodium content.
- Low Sodium: 140 mg or less per serving.
- Reduced Sodium: At least 25% less sodium than the regular product.
- No Salt Added: No salt added during processing, but may still contain naturally occurring sodium.
Cooking Without Salt
Discover alternative seasoning methods to enhance flavor without adding sodium. Herbs, spices, citrus juices, and vinegars can add depth and complexity to dishes.
- Herbs: Basil, oregano, thyme, rosemary, and cilantro.
- Spices: Black pepper, paprika, cumin, turmeric, and garlic powder.
- Citrus: Lemon or lime juice can brighten flavors.
- Vinegars: Balsamic, apple cider, and red wine vinegar for tanginess.
Avoiding High-Sodium Foods
Identify and limit consumption of foods that are naturally high in sodium or contain added salts. Common high-sodium culprits include:
- Processed and packaged foods like chips, crackers, and pretzels.
- Canned soups and broths.
- Deli meats and cured meats such as bacon and sausage.
- Frozen dinners and entrees.
- Restaurant and fast food meals.
Meal Planning Tips
Effective meal planning can significantly reduce sodium intake. Here are some practical tips:
- Choose Fresh or Frozen Vegetables: Instead of canned varieties, which often contain added sodium.
- Opt for Low-Sodium or No-Salt-Added Products: Check labels and select products with reduced sodium.
- Prepare Meals at Home: Cooking from scratch allows you to control the amount of sodium in your food.
- Use Fresh Herbs and Spices: Enhance flavors without relying on salt.
- Rinse Canned Foods: If using canned vegetables or beans, rinse them under water to remove excess sodium.
Substituting Salt in Recipes
Substituting salt with other flavor-enhancing ingredients can maintain taste while reducing sodium intake.
- Use Garlic and Onion: Fresh or powdered garlic and onion can add robust flavors.
- Incorporate Mustard: A small amount of mustard can enhance savory dishes.
- Add Fresh Herbs: Parsley, dill, and cilantro can add freshness to meals.
- Utilize Salt-Free Seasoning Blends: These blends can provide flavor without sodium.
Mindful Eating Practices
Adopting mindful eating practices can help manage sodium intake and promote overall dietary awareness.
- Plan Ahead: Prepare meals in advance to avoid last-minute high-sodium choices.
- Stay Hydrated: Drinking enough water can help balance sodium levels.
- Educate Yourself: Learn about the sodium content in various foods to make informed decisions.
- Portion Control: Even low-sodium foods can contribute to overall sodium intake if consumed in large quantities.
5. Incorporating Potassium
The congestive heart failure diet includes adequate potassium intake to help balance electrolytes and support heart function.
Benefits of Potassium
Potassium helps regulate fluid balance, muscle contractions, and nerve signals, all of which are vital for heart health. It works in opposition to sodium, helping to lower blood pressure and reduce the risk of stroke.
Potassium-Rich Foods
| Food | Potassium Content (mg) | Serving Size |
|---|---|---|
| Bananas | 422 | 1 medium |
| Sweet Potatoes | 337 | 1 medium baked |
| Spinach | 558 | 1 cup cooked |
| Avocados | 485 | 1 medium |
| Oranges | 237 | 1 medium |
| Tomatoes | 292 | 1 cup sliced |
| White Beans | 1,189 | 1 cup cooked |
| Yogurt | 573 | 1 cup |
Balancing Potassium Intake
While potassium is beneficial, it’s essential to maintain it within recommended levels to avoid complications, especially if you’re on certain medications like ACE inhibitors or potassium-sparing diuretics that can increase potassium levels.
- Consult with Healthcare Providers: Before making significant changes to potassium intake, discuss with your doctor or dietitian.
- Monitor Blood Levels: Regular blood tests can help ensure potassium levels remain within a safe range.
- Avoid Excessive Intake: Symptoms of hyperkalemia include muscle weakness, fatigue, and irregular heartbeats.
Potassium and Medications
Certain medications can affect potassium levels. It’s crucial to understand these interactions:
- ACE Inhibitors and ARBs: These medications can increase potassium levels.
- Diuretics: Some, like spironolactone, can retain potassium, while others like furosemide can deplete it.
- Beta-Blockers: May affect potassium balance indirectly.
Practical Tips for Increasing Potassium Intake
- Add Bananas to Breakfast: Slice them over cereal or blend into smoothies.
- Incorporate Leafy Greens: Add spinach or kale to salads, soups, and stir-fries.
- Snack on Nuts and Seeds: Almonds, pistachios, and sunflower seeds are good sources.
- Use Potassium-Rich Ingredients: Include tomatoes in sauces, avocados in sandwiches, and sweet potatoes as side dishes.
Recipes High in Potassium
Here are some delicious recipes that are rich in potassium:
1. Spinach and Avocado Salad
- Ingredients: Fresh spinach, sliced avocados, cherry tomatoes, red onions, and a lemon vinaigrette.
- Instructions: Toss all ingredients in a large bowl and drizzle with dressing.
2. Sweet Potato and Black Bean Tacos
- Ingredients: Roasted sweet potatoes, black beans, corn tortillas, cilantro, and lime wedges.
- Instructions: Assemble sweet potatoes and black beans in tortillas, garnish with cilantro and a squeeze of lime.
3. Yogurt and Banana Smoothie
- Ingredients: Greek yogurt, ripe bananas, honey, and a splash of almond milk.
- Instructions: Blend all ingredients until smooth and serve chilled.
6. Sample Meal Plans

The congestive heart failure diet includes well-balanced meal plans that cater to nutritional needs while managing fluid and sodium intake.
Breakfast
Starting the day with a heart-healthy breakfast sets the tone for nutritious eating:
- Oatmeal with Fresh Berries and Flaxseeds: Cook rolled oats with water or low-fat milk, top with a handful of berries and a sprinkle of ground flaxseeds for added fiber and omega-3s.
- Whole Grain Toast with Avocado and Poached Egg: Mash half an avocado on whole grain toast, add a poached egg for protein, and season with pepper and lemon juice.
- Greek Yogurt with Honey and Sliced Bananas: Combine non-fat Greek yogurt with a drizzle of honey and banana slices for a balanced mix of protein and carbohydrates.
Lunch
Lunch options should be satisfying and low in sodium:
- Grilled Chicken Salad: Mixed greens with grilled chicken breast, cherry tomatoes, cucumbers, and a lemon vinaigrette dressing.
- Quinoa and Black Bean Bowl: Cooked quinoa mixed with black beans, diced bell peppers, corn, and a cilantro-lime dressing.
- Turkey and Avocado Wrap: Sliced turkey breast, avocado, lettuce, and tomato wrapped in a whole wheat tortilla.
Dinner
Dinner should focus on lean proteins and plenty of vegetables:
- Baked Salmon with Steamed Broccoli and Brown Rice: Season salmon with herbs, bake until flaky, and serve with steamed broccoli and a side of brown rice.
- Stir-Fried Tofu with Assorted Vegetables: Sauté tofu with a mix of bell peppers, carrots, snap peas, and a splash of low-sodium soy sauce, served over quinoa.
- Lean Beef Stew: Slow-cook lean beef with carrots, potatoes, green beans, and herbs for a hearty, low-sodium stew.
Snacks
Healthy snacks help maintain energy levels between meals:
- Apple Slices with Almond Butter: Crisp apple slices paired with a tablespoon of almond butter for a sweet and protein-rich snack.
- Carrot and Celery Sticks with Hummus: Crunchy vegetables dipped in low-sodium hummus.
- Mixed Nuts and Dried Fruits: A small handful of unsalted nuts mixed with unsweetened dried fruits for a balanced snack.
Weekly Meal Planner
| Day | Breakfast | Lunch | Dinner | Snacks |
|---|---|---|---|---|
| Monday | Oatmeal with Berries | Grilled Chicken Salad | Baked Salmon with Broccoli | Apple with Almond Butter |
| Tuesday | Whole Grain Toast with Avocado | Quinoa and Black Bean Bowl | Stir-Fried Tofu with Vegetables | Carrot Sticks with Hummus |
| Wednesday | Greek Yogurt with Honey | Turkey and Avocado Wrap | Lean Beef Stew | Mixed Nuts and Dried Fruits |
| Thursday | Scrambled Eggs with Spinach | Lentil Soup with Whole Grain Bread | Grilled Shrimp with Asparagus | Orange Slices |
| Friday | Fruit Smoothie with Flaxseeds | Chicken and Vegetable Stir-Fry | Baked Cod with Sweet Potatoes | Celery Sticks with Peanut Butter |
| Saturday | Pancakes with Fresh Berries | Egg Salad on Whole Wheat Bread | Turkey Meatloaf with Green Beans | Yogurt with Granola |
| Sunday | French Toast with Sliced Bananas | Beef and Vegetable Kebabs | Vegetable Lasagna | Trail Mix |
Adjusting Meal Plans for Special Dietary Needs
Individuals may have unique dietary requirements based on their health status, preferences, and lifestyle. Here are some adjustments:
- Vegetarian/Vegan: Substitute animal proteins with plant-based alternatives like tofu, tempeh, legumes, and quinoa.
- Gluten-Free: Use gluten-free grains such as rice, quinoa, and gluten-free oats.
- Low-Carb: Focus on high-protein and low-carb vegetables, reducing grains and starchy vegetables.
- Allergies: Modify meal plans to exclude allergens like nuts, dairy, or shellfish, using safe alternatives.
Meal Prep and Planning Tips
- Batch Cooking: Prepare large quantities of staples like quinoa, brown rice, and roasted vegetables to use throughout the week.
- Use Storage Containers: Invest in airtight containers to keep prepped meals fresh.
- Label Everything: Clearly label containers with contents and dates to ensure food safety and organization.
- Incorporate Variety: Rotate different proteins, vegetables, and grains to keep meals interesting and nutritionally balanced.
Monitoring Portion Sizes
Managing portion sizes helps control calorie intake and maintain a healthy weight, which is crucial for CHF management.
- Use Measuring Tools: Measuring cups and a kitchen scale can help ensure accurate portion sizes.
- Visual Cues: Compare portion sizes to familiar objects, such as a deck of cards for a serving of meat.
- Mindful Eating: Pay attention to hunger and fullness cues to avoid overeating.
7. Fluid Management
The congestive heart failure diet involves strict fluid management to prevent fluid overload and reduce the strain on the heart.
Daily Fluid Limits
Adhering to prescribed daily fluid limits helps control swelling and maintains optimal heart function. Fluid limits can vary based on individual needs but typically range from 1.5 to 2 liters per day.
- Include All Fluids: This includes water, tea, coffee, juice, soups, and any beverages consumed throughout the day.
- Measure Intake: Use a measuring cup to track fluid consumption accurately.
- Spread Intake: Distribute fluid intake evenly throughout the day to avoid overwhelming the heart at any one time.
Monitoring Fluid Intake
Use tools like fluid diaries or mobile apps to keep track of daily fluid consumption accurately. Consistently monitoring helps in adhering to fluid restrictions and identifying patterns that may need adjustment.
- Fluid Diary: Keep a written log of all fluids consumed, including hidden sources like ice chips or gelatin desserts.
- Mobile Apps: Utilize apps designed for fluid tracking to receive reminders and analyze intake patterns.
- Regular Check-Ins: Review fluid intake with a healthcare provider to ensure adherence and make necessary adjustments.
Hidden Fluids in Foods
Be aware of fluids contained in foods such as soups, ice creams, and fruits to manage total intake effectively. Many foods contain significant amounts of water that contribute to overall fluid consumption.
- Canned Soups and Broths: Opt for low-sodium or broth-free varieties and measure servings carefully.
- Fruits: High-water-content fruits like watermelon and oranges contribute to fluid intake.
- Desserts: Gelatin, sorbet, and other desserts can add to daily fluid limits.
Tips for Staying Hydrated
- Sip Small Amounts: Drink small sips of water throughout the day instead of large quantities at once.
- Use Ice Chips or Frozen Fruit: These can provide hydration without increasing fluid volume significantly.
- Limit High-Fluid-Content Foods: Be mindful of foods that naturally contain more fluids.
- Set Reminders: Use alarms or phone notifications to remind you to take small sips at regular intervals.
Adjusting Fluid Intake During Physical Activity
Physical activity can influence fluid needs. It’s important to balance hydration without exceeding fluid limits:
- Pre-Activity: Drink a small amount of water before exercising to stay hydrated.
- During Activity: Limit fluids and focus on short, frequent sips rather than large quantities.
- Post-Activity: Monitor for any excess fluid retention and adjust intake accordingly.
Signs of Fluid Overload
Recognizing the signs of fluid overload can help in managing CHF effectively:
- Increased Swelling: Noticeable swelling in legs, ankles, or abdomen.
- Weight Gain: Sudden increase in weight due to fluid retention.
- Shortness of Breath: Worsening breathing difficulties.
- Elevated Blood Pressure: Higher readings indicating increased fluid volume.
Strategies to Prevent Fluid Overload
- Follow Fluid Limits: Adhere strictly to prescribed daily fluid allowances.
- Monitor Sodium Intake: Reduce sodium to minimize fluid retention.
- Regular Weigh-Ins: Track weight daily to detect rapid changes indicating fluid buildup.
- Medication Adherence: Take diuretics and other prescribed medications as directed to manage fluid levels.
8. Supplements and Their Role
The congestive heart failure diet may include specific supplements to address nutritional deficiencies and support heart health.
Recommended Supplements
- Omega-3 Fatty Acids: Found in fish oil supplements, they help reduce inflammation and support cardiovascular function.
- Vitamin D: Essential for bone health and may aid in reducing inflammation.
- Magnesium: Supports muscle and nerve function, including the heart muscle.
- Coenzyme Q10: An antioxidant that may improve heart function and reduce oxidative stress.
- Fiber Supplements: Such as psyllium husk, to aid in digestion and cholesterol management.
Supplements to Avoid
Some supplements can interfere with medications or exacerbate CHF symptoms. Always consult with a healthcare provider before starting any new supplement.
- Iron Supplements: Can cause constipation and interfere with certain medications.
- Calcium Supplements: Excessive calcium can lead to calcification of arteries.
- St. John’s Wort: Can interact with heart medications, reducing their effectiveness.
- Excessive Vitamin E: May increase the risk of bleeding, especially when taken with blood thinners.
Consulting Healthcare Professionals
It’s crucial to work with dietitians and doctors to tailor supplement intake to individual health needs and conditions. They can provide guidance on appropriate dosages and monitor for potential interactions.
- Personalized Assessment: Determine specific nutrient deficiencies through blood tests and assessments.
- Professional Recommendations: Receive advice on the best supplements based on individual health profiles.
- Monitoring and Adjustment: Regular follow-ups to adjust supplement regimens as needed.
Natural Sources vs. Supplements
Whenever possible, obtaining nutrients from natural food sources is preferable to supplements, as foods provide a complex matrix of nutrients that work synergistically for optimal health.
- Whole Foods: Emphasize a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Variety: Incorporate a wide range of foods to ensure a broad spectrum of nutrients.
- Supplement Necessity: Only supplement when necessary and under professional guidance.
Potential Benefits of Supplements in CHF
- Improved Heart Function: Supplements like CoQ10 may enhance cardiac efficiency.
- Reduced Inflammation: Omega-3s and vitamin D can help lower inflammatory markers.
- Enhanced Energy Levels: B vitamins and magnesium support energy metabolism.
- Better Nutrient Absorption: Some supplements aid in the absorption of other essential nutrients.
Risks of Unsanctioned Supplements
Taking supplements without proper guidance can lead to adverse effects:
- Over-supplementation: Excessive intake of certain vitamins and minerals can be harmful.
- Interactions with Medications: Supplements can alter the effectiveness of prescribed medications.
- Contamination: Some supplements may contain impurities or undeclared ingredients.
- Misleading Claims: Not all supplements have proven benefits, and some marketing claims may be unfounded.
9. Practical Cooking Tips
The congestive heart failure diet can be both delicious and heart-healthy with the right cooking techniques.
Healthy Cooking Methods
Adopting heart-healthy cooking methods can significantly reduce sodium and unhealthy fat intake while enhancing the natural flavors of foods.
- Grilling: Allows excess fat to drip away from the food, reducing calorie and fat content.
- Steaming: Preserves nutrients in vegetables without adding extra fat or sodium.
- Baking: A versatile method suitable for meats, fish, and vegetables.
- Stir-Frying with Minimal Oil: Quickly cooks ingredients while retaining their texture and nutrients.
- Poaching: Gently cooks foods in liquid, preserving moisture and tenderness without added fat.
Flavor Enhancers
Use herbs, spices, lemon juice, and vinegar to add flavor without relying on salt. These ingredients can transform simple dishes into flavorful meals.
- Herbs: Basil, parsley, cilantro, and dill add fresh flavors.
- Spices: Cumin, paprika, turmeric, and black pepper provide depth and complexity.
- Citrus Juices: Lemon and lime juice brighten flavors and add acidity.
- Vinegars: Balsamic, apple cider, and red wine vinegar add tanginess and balance.
Meal Prepping
Preparing meals in advance ensures adherence to dietary guidelines and saves time during busy weekdays. Here’s how to effectively meal prep:
- Plan Your Meals: Decide on a menu for the week, ensuring a balance of nutrients and adherence to CHF diet guidelines.
- Batch Cook Staples: Prepare large batches of grains, proteins, and roasted vegetables to use in various meals.
- Use Proper Storage: Invest in quality containers that are airtight and suitable for refrigeration or freezing.
- Label and Date: Clearly label each container with the contents and preparation date to ensure freshness and safety.
- Reheat Safely: When reheating, ensure food reaches the appropriate temperature to prevent foodborne illnesses.
Reducing Sodium in Recipes
Experiment with recipes by substituting high-sodium ingredients with low-sodium alternatives. This can help maintain flavor without exceeding sodium limits.
- Use Low-Sodium Broths: Replace regular broth with low-sodium or homemade versions.
- Choose Fresh Over Canned: Fresh vegetables and meats typically contain less sodium than their canned counterparts.
- Limit Processed Ingredients: Reduce the use of processed sauces, dressings, and seasoning mixes.
- Flavor with Acid: Add a splash of vinegar or a squeeze of lemon to enhance flavors naturally.
Smart Ingredient Swaps
Make smart swaps to reduce sodium and unhealthy fats without compromising on taste or texture.
- Salt to Herbs and Spices: Replace salt with a variety of herbs and spices for enhanced flavor.
- Butter to Olive Oil: Use heart-healthy olive oil instead of butter for cooking and baking.
- Regular Pasta to Whole Grain: Opt for whole grain pasta for added fiber and nutrients.
- Full-Fat Dairy to Low-Fat: Choose low-fat or fat-free dairy products to reduce saturated fat intake.
Incorporating Whole Foods
Emphasize whole, unprocessed foods in your cooking to maximize nutrient intake and minimize sodium and unhealthy fats.
- Fruits and Vegetables: Fresh, frozen, or dried without added sugars or salts.
- Whole Grains: Such as brown rice, quinoa, barley, and whole wheat products.
- Lean Proteins: Including skinless poultry, fish, legumes, and tofu.
- Healthy Fats: From sources like avocados, nuts, seeds, and olive oil.
Utilizing Kitchen Gadgets
Modern kitchen gadgets can simplify heart-healthy cooking and make meal preparation more efficient.
- Instant Pot: Speeds up cooking times for stews, beans, and grains without added fat.
- Air Fryer: Allows for crispy textures with significantly less oil.
- Blender/Food Processor: Perfect for making smoothies, purees, and healthy dips like hummus.
- Steamer Basket: Essential for steaming vegetables while preserving nutrients.
10. Dining Out on a CHF Diet
The congestive heart failure diet can be maintained even when dining out with thoughtful planning and communication.
Choosing the Right Restaurant
Select establishments that offer heart-healthy options and are willing to accommodate dietary restrictions. Look for menus that highlight low-sodium and fresh ingredient dishes.
- Research Ahead: Check restaurant menus online before visiting to identify suitable options.
- Opt for Casual Dining: These establishments often provide more flexible menu options compared to fast food or upscale restaurants.
- Seek Recommendations: Ask friends or healthcare providers for restaurant suggestions that cater to heart-healthy diets.
Reading Menus Carefully
Look for dishes that are grilled, baked, or steamed, and inquire about ingredient details to manage sodium and fat intake.
- Look for Descriptive Terms: Words like “grilled,” “roasted,” “steamed,” or “baked” indicate healthier cooking methods.
- Check for Portion Sizes: Be mindful of large portions that can contribute to excess fluid and sodium intake.
- Ask for Ingredient Details: Don’t hesitate to ask the server about how dishes are prepared and what ingredients are used.
Making Special Requests
Don’t hesitate to ask for modifications such as no added salt, dressing on the side, or substituting high-sodium sides with vegetables.
- No Added Salt: Request that your meal be prepared without added salt to control sodium intake.
- Dressing on the Side: This allows you to control the amount of dressing used, reducing sodium and fat intake.
- Substitute Sides: Replace high-sodium sides like fries or mashed potatoes with steamed vegetables or a side salad.
- Whole Grain Options: Ask if whole grain alternatives are available for breads, pastas, or rice.
Portion Control
Be mindful of portion sizes to avoid overeating, which can lead to fluid retention and increased heart strain.
- Share Dishes: Order shared appetizers or entrees to split portions.
- Request Half Portions: Ask if half-sized portions are available.
- Take Half Home: Don’t hesitate to ask for a to-go box and save half your meal for later.
- Listen to Your Body: Eat slowly and stop when you feel satisfied, not overly full.
Healthy Beverage Choices
Select beverages that align with your fluid management goals. Avoid sugary drinks and excessive caffeine.
- Water: The best choice for hydration without added calories or sodium.
- Herbal Teas: Offer flavor without caffeine or sugar.
- Sparkling Water: Provides a fizzy alternative without added sugars.
- Limit Alcohol: Alcohol can interfere with medications and exacerbate CHF symptoms.
Dining Etiquette for CHF Management
Adopting mindful dining practices can help maintain your CHF diet while enjoying meals out.
- Plan Ahead: Know what you’ll eat before arriving at the restaurant to avoid impulsive choices.
- Communicate Clearly: Politely inform the server about your dietary restrictions and preferences.
- Stay Hydrated: Drink fluids according to your prescribed limits, even when enjoying a meal out.
- Enjoy Your Meal: Focus on savoring the flavors and textures, which can enhance satisfaction and reduce the urge to overeat.
Managing Social Situations
Social gatherings and events can present challenges for maintaining a CHF diet. Here are strategies to navigate these situations:
- Bring Your Own Dish: If possible, contribute a heart-healthy dish to share.
- Scout the Menu: Upon arrival, take a moment to review the menu and choose options that fit your dietary needs.
- Focus on the Company: Prioritize social interactions over the food, which can help in making mindful eating choices.
- Set Personal Boundaries: Politely decline offers of high-sodium or unhealthy foods without feeling guilty.
Maintaining Consistency
Consistency is key in managing CHF through diet. Even occasional deviations can impact your health, so it’s important to stay committed.
- Stay Informed: Continuously educate yourself about heart-healthy eating and stay updated with new dietary guidelines.
- Seek Support: Engage with support groups or communities for motivation and accountability.
- Monitor Progress: Keep track of your health metrics and dietary adherence to identify areas for improvement.
- Celebrate Successes: Acknowledge and reward yourself for maintaining a heart-healthy diet.
11. Frequently Asked Questions
1. How much sodium should I consume daily on a CHF diet?
Most CHF patients are advised to limit their sodium intake to less than 2,000 mg per day. However, individual recommendations may vary based on specific health conditions and doctor’s advice.
2. Can I eat out while following a congestive heart failure diet?
Yes, with careful planning and communication. Choose restaurants that offer heart-healthy options, request modifications, and be mindful of portion sizes and sodium content.
3. Are there specific foods I should avoid entirely?
It’s best to limit or avoid processed and high-sodium foods such as canned soups, deli meats, fast food, and packaged snacks. Also, limit sugary and high-fat foods to maintain overall heart health.
4. Do I need to take vitamin supplements?
Not necessarily, unless recommended by your healthcare provider. It’s preferable to obtain nutrients from a balanced diet. Supplements should only be taken under professional guidance to avoid interactions and over-supplementation.
5. How can I manage fluid intake during physical activities?
Balance hydration by sipping small amounts of water before, during, and after exercise. Avoid large quantities at once and consult with your healthcare provider to tailor fluid management strategies to your activity level.
6. What are some low-sodium seasoning alternatives?
Herbs, spices, lemon or lime juice, vinegar, garlic, and salt-free seasoning blends are excellent alternatives to enhance flavor without adding sodium.
7. How often should I monitor my weight?
Daily weigh-ins are recommended to quickly detect fluid retention. Consistent monitoring helps in making timely dietary and medication adjustments as needed.
8. Can I include occasional treats in my CHF diet?
Yes, moderation is key. Choose healthier alternatives to traditional treats, such as low-sodium versions of your favorite snacks or desserts, and limit portion sizes to maintain overall dietary balance.
9. How does a CHF diet affect my energy levels?
A balanced CHF diet provides essential nutrients that support energy metabolism. Adequate protein, healthy fats, and complex carbohydrates help maintain steady energy levels throughout the day.
10. What should I do if I experience symptoms despite following the diet?
If you notice worsening symptoms like increased shortness of breath, swelling, or fatigue despite adhering to your diet, contact your healthcare provider promptly. Adjustments to your dietary plan or medications may be necessary.
12. Conclusion
The congestive heart failure diet is a cornerstone in managing CHF effectively. By adhering to dietary guidelines that emphasize low sodium, balanced electrolytes, and nutrient-rich foods, individuals can significantly improve their quality of life and reduce the risk of hospitalization.
Key Takeaways
- Importance of Diet: A well-planned diet can alleviate symptoms and support overall heart health.
- Monitor Sodium and Fluid Intake: Critical for preventing fluid retention and managing blood pressure.
- Incorporate Essential Nutrients: Potassium, magnesium, fiber, and omega-3 fatty acids play vital roles in heart health.
- Plan and Prepare: Effective meal planning and preparation can make adhering to the CHF diet more manageable.
- Seek Professional Guidance: Collaborate with healthcare providers and dietitians to tailor the diet to individual needs.
Empowering Yourself Through Knowledge
Educating yourself about CHF and the role of diet in its management empowers you to make informed decisions about your health. Staying informed, seeking support, and maintaining consistency are essential steps toward living well with congestive heart failure.
Maintaining a Positive Outlook
Managing CHF through diet is a proactive approach that can lead to meaningful improvements in health and well-being. Embrace the journey with a positive mindset, celebrate your progress, and stay committed to your heart-healthy lifestyle.
References and Further Reading




