Intermittent Fasting for IBS: A Comprehensive Guide
1. Introduction to Intermittent Fasting and IBS
Intermittent fasting for IBS has gained significant attention as a potential strategy to manage symptoms of Irritable Bowel Syndrome (IBS). IBS is a common gastrointestinal disorder characterized by symptoms like abdominal pain, bloating, and altered bowel habits. Traditional management strategies often include dietary modifications, stress management, and medication. However, integrating intermittent fasting into an IBS management plan offers a novel approach that many are finding beneficial.
This comprehensive guide delves into how intermittent fasting can be utilized to alleviate IBS symptoms, the mechanisms behind its effectiveness, different fasting protocols suitable for IBS sufferers, and practical tips for implementation. By understanding the relationship between intermittent fasting and IBS, individuals can make informed decisions to improve their quality of life.
2. Benefits of Intermittent Fasting for IBS
Intermittent fasting for IBS offers several benefits that can help manage and potentially reduce the severity of IBS symptoms. Understanding these benefits is crucial for anyone considering this approach as part of their treatment plan.
- Reduced Inflammation: Intermittent fasting has been shown to decrease systemic inflammation, which can alleviate the inflammatory responses associated with IBS.
- Improved Gut Health: Fasting periods allow the gut to rest and repair, promoting a healthier microbiota balance, which is essential for individuals with IBS.
- Enhanced Digestive Efficiency: By regulating meal times, intermittent fasting can improve digestive processes, reducing symptoms like bloating and gas.
- Weight Management: Maintaining a healthy weight can lessen the strain on the digestive system, potentially reducing IBS symptoms.
- Stress Reduction: Intermittent fasting can influence stress hormones, helping to manage the stress that often exacerbates IBS.
These benefits collectively contribute to a holistic approach in managing IBS, addressing both the physical and psychological aspects of the condition.
3. How Intermittent Fasting Affects IBS Symptoms
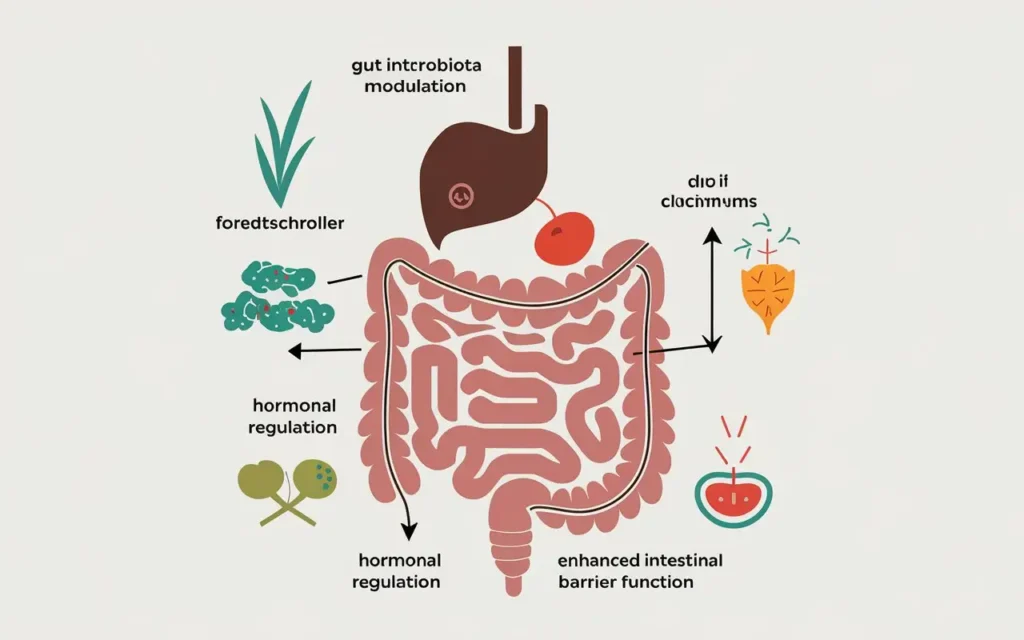
Intermittent fasting for IBS works through several physiological mechanisms that directly impact the symptoms and underlying causes of Irritable Bowel Syndrome.
3.1. Gut Microbiota Modulation
Intermittent fasting can alter the composition of the gut microbiota, promoting the growth of beneficial bacteria while reducing harmful strains. A balanced microbiome is crucial for digestive health and can significantly reduce IBS symptoms.
3.2. Enhanced Intestinal Barrier Function
Fasting periods allow the intestinal lining to repair and strengthen, reducing permeability (often referred to as “leaky gut”). This enhanced barrier function can prevent the translocation of toxins and reduce inflammation.
3.3. Hormonal Regulation
Intermittent fasting influences hormones such as cortisol and insulin, which play roles in stress response and metabolic processes. Balanced hormone levels can mitigate the stress-related triggers of IBS.
3.4. Autophagy and Cellular Repair
During fasting, the body undergoes autophagy, a process where cells remove damaged components and regenerate. This cellular repair can improve overall gut health and functionality.
3.5. Reduction of Gastrointestinal Transit Time
Intermittent fasting can help regulate the speed at which food moves through the digestive tract. Proper transit time can reduce symptoms like diarrhea and constipation, common in IBS.
4. Types of Intermittent Fasting Suitable for IBS

Intermittent fasting for IBS can be approached through various fasting protocols. Selecting the right type is essential to ensure that it complements your IBS management without exacerbating symptoms.
4.1. Time-Restricted Eating (TRE)
TRE involves limiting food intake to a specific window each day, typically 8-10 hours. For example, eating between 10 AM and 6 PM. This method is often easier to adhere to and can help regulate meal times, benefiting IBS sufferers.
4.2. 5:2 Fasting
The 5:2 method allows normal eating for five days of the week while restricting calorie intake to about 500-600 calories on two non-consecutive days. This approach can provide the benefits of fasting without daily restrictions, which might be preferable for some with IBS.
4.3. Alternate-Day Fasting (ADF)
ADF involves alternating between days of regular eating and days of fasting or very low-calorie intake. While effective, this method may be challenging for IBS sufferers due to the potential for increased stress on the digestive system.
4.4. Extended Fasting
Extended fasting periods, such as 24-48 hours, are less commonly recommended for IBS due to the higher risk of triggering symptoms. However, occasional extended fasts under medical supervision may offer benefits for some individuals.
4.5. Modified Fasting
Modified fasting involves consuming a reduced number of calories or specific types of foods during fasting periods. This approach can help maintain nutrient intake while still reaping the benefits of fasting, making it suitable for those with IBS.
5. Implementing Intermittent Fasting in Your IBS Management Plan
Intermittent fasting for IBS requires careful planning and consideration to ensure that it effectively complements your existing management strategies. Here’s how to integrate intermittent fasting into your IBS regimen:
5.1. Consult with Healthcare Professionals
Before starting intermittent fasting, it’s crucial to consult with a gastroenterologist or a dietitian who understands your medical history and can provide personalized advice.
5.2. Start Gradually
Begin with a more lenient fasting schedule, such as 12-hour fasting periods, and gradually increase the fasting window as your body adapts.
5.3. Monitor Your Symptoms
Keep a detailed diary of your symptoms, dietary intake, and fasting periods. This will help identify patterns and adjust your fasting schedule accordingly.
5.4. Stay Hydrated
Ensure adequate hydration during fasting periods by drinking water, herbal teas, and other non-caffeinated beverages to support digestive health.
5.5. Prioritize Nutrient-Dense Foods
During eating windows, focus on consuming nutrient-dense, fiber-rich foods that support gut health and reduce IBS symptoms.
5.6. Listen to Your Body
Pay attention to how your body responds to intermittent fasting. If you notice worsening symptoms, it may be necessary to adjust your fasting schedule or discontinue the practice.
5.7. Combine with Other Management Strategies
Integrate intermittent fasting with other IBS management techniques such as stress reduction, regular exercise, and medication adherence for optimal results.
6. Dietary Considerations While Practicing Intermittent Fasting for IBS

Intermittent fasting for IBS is most effective when combined with dietary choices that support digestive health. Here are key considerations to keep in mind:
6.1. Low FODMAP Diet
Adhering to a low FODMAP diet during eating periods can help reduce IBS symptoms by eliminating fermentable carbohydrates that trigger digestive distress.
6.2. Balanced Macronutrients
Ensure a balance of proteins, healthy fats, and complex carbohydrates to provide sustained energy and support gut health.
6.3. High Fiber Intake
Incorporate soluble fiber sources such as oats, bananas, and carrots to aid digestion and prevent constipation without exacerbating IBS.
6.4. Probiotics and Prebiotics
Include probiotic-rich foods like yogurt and prebiotic foods like asparagus to enhance gut microbiota balance, which can alleviate IBS symptoms.
6.5. Hydration
Maintain adequate fluid intake to support digestion and prevent dehydration, especially during fasting periods.
6.6. Avoid Trigger Foods
Identify and avoid foods that trigger your IBS symptoms, such as caffeine, alcohol, and spicy foods, to minimize discomfort during intermittent fasting.
6.7. Mindful Eating
Practice mindful eating by chewing thoroughly and eating slowly to improve digestion and reduce IBS flare-ups.
7. Potential Risks and How to Mitigate Them
Intermittent fasting for IBS can offer significant benefits, but it also comes with potential risks that need to be carefully managed to ensure safety and effectiveness.
7.1. Nutrient Deficiencies
Prolonged fasting periods may lead to inadequate nutrient intake. Mitigate this by focusing on nutrient-dense foods during eating windows and, if necessary, supplementing under professional guidance.
7.2. Increased Stress Levels
Fasting can be a physical stressor. To mitigate stress, combine intermittent fasting with stress-reduction techniques such as meditation, yoga, or deep-breathing exercises.
7.3. Exacerbation of Symptoms
Some individuals may experience worsening of IBS symptoms due to changes in meal patterns. Monitor your body’s response and adjust your fasting schedule as needed.
7.4. Disordered Eating Patterns
There’s a risk of developing unhealthy eating behaviors. Ensure that intermittent fasting is approached as a structured health strategy rather than a diet, and seek professional support if necessary.
7.5. Hypoglycemia
Fasting can cause low blood sugar levels, especially in individuals with diabetes or other metabolic conditions. Monitor blood sugar levels and consult with a healthcare provider before starting intermittent fasting.
7.6. Dehydration
Inadequate fluid intake during fasting periods can lead to dehydration. Ensure regular hydration by drinking water and other non-caffeinated, non-sugary beverages.
7.7. Social and Lifestyle Challenges
Fasting schedules may interfere with social activities and daily routines. Plan your fasting periods around your lifestyle to minimize disruptions and maintain social connections.
8. Expert Advice and Recommendations
Intermittent fasting for IBS is a strategy that should be personalized based on individual health profiles and under professional guidance. Here are some expert recommendations to consider:
8.1. Consult a Registered Dietitian
A dietitian can help tailor an intermittent fasting plan that aligns with your nutritional needs and IBS management goals.
8.2. Gradual Implementation
Start with shorter fasting periods and gradually increase as your body adapts, reducing the risk of adverse reactions.
8.3. Monitor and Adjust
Regularly assess your symptoms and overall well-being, making adjustments to your fasting schedule as necessary in consultation with your healthcare provider.
8.4. Focus on Quality Nutrition
Prioritize high-quality, whole foods during eating windows to support overall health and mitigate IBS symptoms.
8.5. Incorporate Stress Management Techniques
Utilize stress reduction strategies to complement intermittent fasting, as stress is a known trigger for IBS flare-ups.
8.6. Stay Informed
Keep abreast of the latest research on intermittent fasting and IBS to make informed decisions about your health management strategies.
8.7. Seek Support
Engage with support groups or communities of individuals who are also practicing intermittent fasting for IBS to share experiences and strategies.
9. Personal Stories: Success with Intermittent Fasting for IBS

Intermittent fasting for IBS has been a transformative strategy for many individuals. Here are some personal stories highlighting the positive impacts and experiences of those who have integrated fasting into their IBS management.
9.1. Sarah’s Journey to Symptom Relief
Sarah struggled with chronic IBS symptoms for years, trying various diets and medications with limited success. Upon adopting a 16:8 intermittent fasting schedule, she noticed a significant reduction in bloating and abdominal pain within a few weeks. By focusing on nutrient-dense foods during her eating window, Sarah was able to maintain her energy levels and improve her overall digestive health.
9.2. Michael’s Path to Better Gut Health
Michael found that traditional dietary approaches did not fully alleviate his IBS symptoms. Introducing intermittent fasting allowed his digestive system regular periods of rest, leading to improved gut microbiota balance. Over time, Michael experienced fewer episodes of diarrhea and constipation, enhancing his quality of life.
9.3. Emily’s Experience with Stress Reduction
For Emily, stress was a major trigger for her IBS flare-ups. Incorporating intermittent fasting into her routine not only helped regulate her meal times but also provided a structured approach that reduced her overall stress levels. Combined with mindfulness practices, Emily saw a marked improvement in her symptom management.
9.4. John’s Balanced Approach
John combined intermittent fasting with a low FODMAP diet to manage his IBS. This dual approach allowed him to address both dietary triggers and improve his digestive system’s resilience. John’s success underscores the importance of a holistic strategy in managing IBS.
9.5. Lisa’s Story of Consistency and Patience
Lisa emphasizes the role of consistency in her intermittent fasting journey. By adhering to a consistent fasting schedule and making mindful food choices, she was able to stabilize her bowel movements and reduce the unpredictability of her IBS symptoms. Lisa’s story highlights the importance of patience and persistence in achieving long-term benefits.
10. Conclusion and Next Steps
Intermittent fasting for IBS presents a promising approach to managing Irritable Bowel Syndrome symptoms through various physiological and lifestyle mechanisms. By understanding the benefits, mechanisms, and best practices for implementation, individuals can make informed decisions to enhance their digestive health and overall well-being.
To embark on this journey, consider the following next steps:
- Consult with a healthcare professional to determine if intermittent fasting is suitable for your specific condition.
- Choose a fasting protocol that aligns with your lifestyle and IBS management needs.
- Focus on a balanced, nutrient-dense diet during eating periods to support gut health.
- Monitor your symptoms and adjust your fasting schedule as necessary.
- Incorporate stress management techniques to complement your fasting regimen.
- Stay informed and seek support from communities and professionals.
By taking a thoughtful and personalized approach, intermittent fasting can be a valuable tool in your IBS management toolkit, contributing to a healthier and more comfortable life.
References and Further Reading




